Neurological Exam
DEFINITION
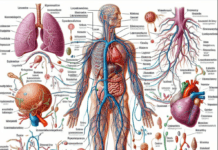
A neurological exam—also called a neurologic or neuro exam—is an evaluation of the nervous system, including the brain, spinal cord, the 12 cranial nerves that come from the brain, and the nerves that come from the spinal cord.
A neurological exam uses observation and simple tests to assess motor and sensory skills and mental status.
Motor skills include reflexes, muscle strength, eye, mouth movement, coordination, balance, and gait. Sensory skills include hearing and speech, vision, taste, and smell.
Mental status includes alertness, awareness of and interaction with one’s environment, and mood and behavioral changes.
DESCRIPTION
A neurological exam is neither invasive nor painful. It can be performed in a physician’s office and involves only simple instruments such as a reflex hammer, tuning fork, needles, a light, and an ophthalmoscope.
The simplest aspects of a neurological exam involve observing a patient’s gait and coordination and whether the eyelids are drooping.
However, some specialized exams may require a neurologist to perform the tests and analyze the results.
The extent of a neurological exam depends on the symptoms being evaluated and the patient’s age and medical condition.
For some injuries, it may be necessary to repeat portions of the exam after swelling from the injury has decreased.
In certain cases, such as after a stroke, neurological exams may be repeated at regular intervals to monitor the condition.
A neurological exam focuses on the following:
- motor skills, including reflexes, muscle strength, head, and facial movements, coordination, balance, and gait
- sensory skills
- mental status and basic cognitive skills
- cranial nerves
Motor nerve function—intense tendon reflexes—are central to a neurological exam. Deep tendon reflexes, also known as muscle stretch reflexes, are tendon responses to stimuli.
Normally, tapping specific areas of tendons with a soft rubber hammer causes the muscle fibers to contract.
The physician taps various points with a reflex hammer and observes any decrease in responsiveness.
The Babinski reflex is an important component of motor system evaluation.
In patients over the age of two, stroking or scratching the outer side of the sole in a heel-to-toe direction normally causes the toes to curl downward.
A brain or spinal cord injury is indicated by the toes fanning upward.
The physician examines the patient’s muscles for atrophy (shrinkage), twitching, or abnormal movements.
Tests may be performed to evaluate the strength of all major muscle groups.
Specific tests may include:
- squeezing fingers
- using the arms and legs to push and pull against the physician’s hands
- passive movement of the joints by the physician and active movement by the patient
Head and facial movement tests may include:
- touching various areas of the face
- biting down
- swallowing
- smiling, grimacing, moving the cheeks, and baring the teeth
- tongue movement
- testing the gag reflex using a tongue blade
- head movements such as turning side to side against mild resistance
- shrugging the shoulders
Tests of coordination, balance, and gait may include:
- observation of a patient’s walk and general coordination
- moving one’s finger back and forth between one’s nose and the examiner’s finger, touching the tip of each
- tapping one’s fingers together rapidly in a coordinated manner
- moving one’s hands back and forth on top of one another as smoothly as possible
- rubbing one heel smoothly over the other shin
- drawing a spiral
- touching a finger to one’s nose with the eyes closed
- balancing with the feet together and eyes closed
- standing with the eyes closed while being gently pushed to one side
- heel-to-toe walking in a straight line
- walking on one’s toes
- turning abruptly
- running, hopping, skipping, or jumping
- evaluation of any functional limitations, such as difficulty writing or holding a cup or utensil
Sensory tests may include:
- hearing tests using a ticking watch or a tuning fork
- clarity, fluency, and coherence of speech
- vision tests
- examining the eye with a special light to evaluate the optic nerve
- using light to evaluate pupil size reflex
- evaluating eye movement by having the patient follow a light or the examiner’s finger in various directions with the eyes
- identifying various tastes—such as sweet, sour, and bitter—on the back of the tongue
- identifying different smells with the eyes closed
- identifying objects and sensations—such as sharp or dull—as the physician touches parts of the patient’s body with a finger, sharp object, cotton ball, paintbrush, dull needle, tuning fork, or alcohol swab
- identifying numbers or letters traced on the body
- using pinpricks to test a patient’s pain response on different parts or opposite sides of the body
- using cold or warm objects to test temperature sensations
- sensing a position by identifying the direction in which the examiner is moving a part of the patient’s body, such as a big toe
Evaluating mental status is particularly important when other parts of a neurological exam yield normal results.
In certain instances, small changes in memory or other intellectual abilities are the only indication of a problem.
Evaluating mental skills can also be useful for determining a course of treatment and making a prognosis.
Mental status tests may involve observing the patient for the following:
- consciousness or awareness of and responsiveness to the environment and the senses
- ability to follow simple and complex directions
- orientation concerning time, place, and person, such as knowing the current time and date and the current president
- attentiveness
- ability to appropriately answer simple but detailed questions
- ability to read and write
- intellectual capacity, including comprehension, insight, and judgment
- solving simple mathematical problems
- copying a three-dimensional drawing
- drawing a clock with the numbers and hands placed appropriately
- abstract reasoning such as explaining the meaning of common sayings
- memory, such as repeating sentences or a list of objects used early in the exam or describing yesterday’s break-fast or what happened on the last holiday
- appearance, mood, and general behavior
- with an infant, observing the child’s interaction with parents
Specific components of a neurological exam evaluate the function of each of the 12 cranial nerves:
- cranial nerve I—the olfactory nerve
- cranial nerve II—the optic nerve
- cranial nerve III—the oculomotor nerve responsible for pupil size and eye movement
- cranial nerve IV—the trochlear nerve involved in eye movement
- cranial nerve V—the trigeminal nerve, which has various functions, including the ability to feel the face and inside the mouth and move muscles involved in chewing
- cranial nerve VI—the abducens nerve involved in eye movement
- cranial nerve VII—the facial nerve, which has various functions, including taste and movement
- cranial nerve VIII—the acoustic nerve
- cranial nerve IX—the glossopharyngeal nerve involved in taste
- cranial nerve X—the vagus nerve involved in swallowing, gag reflex, and aspects of taste and speech
- cranial nerve XI—the accessory nerve involved in moving the head and shoulders
- cranial nerve XII—the hypoglossal nerve responsible for tongue movement
A newborn or infant neurological exam evaluates reflexes or automatisms, each of which disappears at a certain stage of normal development.
Those reflexes include, but are not limited to, the following:
- blinking—closing the eyes in response to a bright light
- Babinski reflex—the toes extending upward as an infant’s foot is stroked
- crawling—infants making crawling motions when placed on their stomach
- Moro reflex—infants throwing out their arms, opening their hands, and throwing back their heads when startled or moved rapidly
- palmar and plantar grasps—infants’ fingers and toes curling around a nearby finger
- startle reflex—infants extending and flexing the arms with the hands fisted in response to loud noise
Measurement of head circumference is also part of a neurological exam in infants and younger children.
PURPOSE
Neurological exams are performed for a variety of purposes:
- as part of a complete physical exam
- as part of a newborn physical exam
- to assess or follow the effects of a head or spine congenital disability
- for the diagnosis of a wide variety of diseases and conditions
- to follow the progression or management of a disease or condition
- to monitor an injury to the head, neck, or back
- to monitor recovery following brain surgery
Neurological exams are routine in some sports, most notably preseason exams for all National Football League players to provide a baseline in case of concussion.
A neurological exam can reveal signs of increased intracranial pressure or decreased brain function.
In addition to concussions, neurological exams are performed on patients with any of the following symptoms:
- fatigue
- headaches
- blurred vision
- fever of unknown origin
- numbness or tingling in the arms or legs
- decreased arm or leg movement
- tremor
- uncontrollable jerky body movements
- problems with balance or coordination
- behavioral changes
KEY TERMS
Automatism— An automatic action or reflex.
Babinski reflex— A reflex movement by the big toe when the sole is tickled; an upward response is normal in infancy but indicates central nervous system damage in older children and adults.
Moro reflex— A reflex startle reaction in infants; the arms and legs move away from the body and to the side and are then drawn together.
Ophthalmoscope— An instrument for viewing the interior of the eye.
Stroke— A sudden diminishment of consciousness, sensation, or voluntary movement caused by a rupture or clot in a blood vessel in the brain.
Tendon reflex— A reflex reaction, such as a knee jerk, in which a light blow to the tendon causes the muscle to contract.
A neurological exam is often one of the first procedures in the diagnosis of many diseases and conditions, including the following:
- central nervous systems (CNS) infections, such as encephalitis and meningitis
- stroke
- transient ischemic attacks—in which the exam results may be abnormal during the episode but normal immediately afterward
- bleeding in the brain
- spinal cord injuries
- carotid artery disease
- peripheral neuropathy
- alcoholic neuropathy
- erectile dysfunction
- brain and spinal cord tumors, including pituitary tumors and primary CNS lymphomas
- nasopharyngeal cancer
- brain abscesses
- brain herniation
- epilepsy
- cerebral palsy
- dementia
- Alzheimer’s disease
- Parkinson’s disease
- Huntington’s disease
- multiple sclerosis
- myasthenia gravis—a muscle weakness disorder
- neurological complications of HIV/AIDS
- systemic lupus erythematosus, a chronic inflammatory
- autoimmune disease
- amyotrophic lateral sclerosis (ALS)
- congenital toxoplasmosis
- craniosynostosis, a congenital disability in which one or more sutures on an infant’s head close too early
- mitochondrial diseases
- motor neuron diseases
- metabolic diseases of muscle
RESULTS
A neurological exam is a relatively simple, quick, and inexpensive means of identifying a wide range of neurological abnormalities.
A simple neurological exam is superior to expensive computed tomography (CT) scans for diagnoses in many cases.
Neurological problems and nervous system damage can cause delays in infant and child development and functioning:
Early diagnosis of problems using a neurological exam can help identify the cause and decrease the likelihood of long-term complications.
PRECAUTIONS
Precautions concerning a neurological exam include:
- The exam requires skill and patience on the part of the physician.
- Importantly, the exam requires the patient’s cooperation.
- Responses can be affected by the wakefulness, awareness, and alertness of the patient, so the mental status portion of a neurological exam is usually performed early on.
- The sensory exam should be repeated for accuracy. Aftercare
AFTERCARE
There are no special preparations or risks involved in a neurological exam.
However, abnormal results may require further procedures such as a CT scan, magnetic resonance imaging (MRI), x-rays, or laboratory tests.
The patients can be referred to a neurologist or other specialist.
Resources
Biller, Jose, et al. DeMyer’s The Neurologic Examination: A Programmed Text, 6th ed. New York: McGraw-Hill Professional, 2011.
healthcommunities.com. “What Is a Neurological Exam?” http://www.healthcommunities.com/brain-nerve-tests/what-is-a-neuro-exam.shtml (accessed November 5, 2019).
Larsen, Paul D., and Suzanne S. Stensaas. “Neurologic Exam: An Anatomic Approach.” Neurologic Exams and Videos: An Anatomic Approach. http://library.med.utah.edu/neurologicexam/html/home_exam.html (accessed November 5, 2019).
Medscape. “Neurological History and Exam.” http://emedicine.medscape.com/article/1147993-overview (accessed November 5, 2019).
American Brain Tumor Association, 2720 River Rd., Des Plaines, IL 60018, (847) 827-9910, (800) 886-2282, (847) 827-9918 [email protected], http://www.abta.org.
National Institute of Neurological Disorders and Stroke (NINDS), NIH Neurological Institute, PO Box 5801, Bethesda, MD 20824, (301) 496-5751, (800) 352-9424, http://www.ninds.nih.gov.