Acid Reflux Symptoms
Acid Reflux Symptoms
Between 25 percent to 40 percent of Americans of all ages suffer from acid reflux symptoms.
An estimated 20 percent of adults experience gastroesophageal reflux disease weekly or daily — commonly called GERD or referred to as heartburn, a more severe case of acid reflux.
(1) Why do so many suffer from these agitating, often persistent, symptoms of indigestion?
As you’ll learn, there are many common causes of GERD and acid reflux, including pregnancy, Hiatal hernias, eating an unhealthy diet, and an imbalance of stomach acid.
These can result in acid regurgitation that triggers unpleasant acid reflux symptoms, such as burning or belching. (2)
At the root of acid reflux is a dysfunction of the lower esophageal sphincter, which is supposed to close as soon as food passes.
However, if it doesn’t close all the way, acid can creep up from the lower in the digestive system and begin to cause an array of problems.
If it’s not treated properly, long-term acid reflux can cause severe damage.
Easing acid reflux or GERD symptoms temporarily with medications or over-the-counter drugs is usually not a cure — it’s only a way to offer some relief as symptoms are suppressed in the short-term.
Ironically, these medications may cause new or worsened symptoms, depending on how your body reacts to them.
If you’ve been relying on over-the-counter and/or prescriptions to ease pain and discomfort, you might be familiar with some of the notorious side effects associated with their use, which include headaches, muscle cramps, rapid heart rate, and more digestive upset.
Below you’ll find information related to natural remedies for managing acid reflux symptoms, providing you with a much better understanding of what causes this type of digestive dysfunction to begin with and how it can finally come to an end.
In addition to lowering acid reflux symptoms, the same treatments can also usually help manage related issues, such as GERD symptoms.
Acid Reflux Symptoms
The most common acid reflux and GERD symptoms include: (3)
- Heartburn
- Bitter taste in your mouth, periodically or (for some people) throughout the day (some people taste regurgitated food or sour liquid at the back of their mouths/throats)
- Waking up in the middle of the night feeling like you’re choking or coughing
- Dry mouth
- Gum irritation, including tenderness and bleeding
- Bad breath
- Regurgitation of acidic foods
- Bloating after meals and during bouts of symptoms
- Nausea
- Bloody vomiting (a possible sign of damage in the lining of the esophagus)
- Black stools
- Belching, gassiness, burping, and flatulence after meals
- Hiccups that are difficult to stop
- Difficulty swallowing (a possible sign of narrowing esophagus)
- Unexpected weight loss
- Increased discomfort when bending over or lying down
- Hoarseness upon waking or throughout the day
- Chronic throat irritation, soreness, and dryness
Complications
If you experience ongoing regurgitation of acid — because you don’t respond well to medications or don’t take steps to treat the root causes, scarring tissue in the lower esophagus can narrow the esophagus raises the risk for other problems.
Research shows that long-term complications associated with untreated symptoms of acid reflux include Barrett’s esophagus (a serious complication of GERD), cancer of the esophagus, sleep-related problems, and chronic coughs. (4)
As the rate of acid reflux has risen steadily over the past decade, so have related complications.
The American Cancer Society estimates that in 2017, nearly 17,000 new esophageal cancer cases were diagnosed in the U.S., and almost 16,000 Americans died of the disease.
There are also side effects and complications possible due to acid reflux medications, including prescription and even over-the-counter drugs. I’ll touch on that shortly.
Causes and Risk Factors
Contrary to popular belief (and what many pharmaceutical companies say in advertisements), acid reflux symptoms are not caused by too much acid in the stomach.
In fact, it is now believed by many that low stomach acid often causes symptoms.
Acid reflux is caused by acid rising to the esophagus, the tube that connects the throat and stomach.
Acid enters the esophagus because of a leaky valve, and there are various reasons this happens.
The esophageal valve that connects the esophagus and stomach cannot shut properly, and gastric juices end up “sneaking up the pipe.”
Then without proper levels of acid in the stomach, digestion is altered, often causing unpleasant symptoms.
While everyone’s gut is different, and we all have different food sensitivities and acid reflux triggers, some repeat offenders seem to contribute to many cases of acid reflux or GERD. (5)
Causes and risk factors associated with acid reflux and GERD include:
Inflammation: Studies have found that high inflammation levels are linked to GERD development because they cause tissue damage and dysfunction in the esophagus.
(6) Inflammation left to fester is also a factor in esophageal cancer development, a known complication of acid reflux. (7)
Hiatal Hernia: Hiatal hernias can cause unpleasant symptoms of acid reflux. The diaphragm helps separate the stomach from the chest.
A hiatal hernia happens when the stomach’s upper part protrudes above the diaphragm, allowing acid to escape. These hernias are associated with most, but not all, cases of GERD. (8)
Carbohydrate malabsorption: More and more evidence points to the link between the poor digestion of carbohydrates and GERD.
In the book “Heartburn Cured,” Dr. Norm Robillard argues that we target some incorrect trigger foods when treating GERD nutritionally and that more focus should be on eliminating excess carbohydrates.
The mechanisms behind this are somewhat complex, but to sum it up: research seems to reflect that acid reflux and GERD are probably exacerbated by too much intra-abdominal pressure (gas throughout the intestines).
(9) Robillard and other sources believe this pressure results from bacterial overgrowths, such as SIBO, and malabsorption of carbohydrates.
The root of this pressure may ultimately trace back to the low stomach acid of those suffering from acid reflux. (10)
Underdeveloped digestive system: Babies can develop acid reflux or GERD due to an underdeveloped digestive system. GERD in babies usually self-corrects by the age of 1.
Aging: Many aging and elderly members of the American population lack the appropriate amount of stomach acid needed to fully digest their food, often considered a side effect of taking antacids regularly and/or malnutrition.
(11) This is true especially for those older individuals with H. pylori infections, which ultimately leads to atrophic gastritis, an inflammation of the gastric mucosa within the stomach. (12, 13)
One complication of acid reflux and GERD in elderly patients is that their symptoms present differently than younger people suffering the same issues.
Repeated reflux eventually leads to an inability to recognize the severity of acid in the esophagus, which is why some older people don’t recognize symptoms of acid reflux. However, they may be suffering from serious complications like erosive esophagitis or Barrett’s esophagus.
It is not uncommon for doctors to find that GERD is the root cause of serious symptoms in the elderly like chest pain, other heart symptoms, and gastrointestinal bleeding. (14)
Pregnancy: When a woman is pregnant, the fetus can put extra pressure on the esophageal valve, causing the release of acid and symptoms of acid reflux.
Elevating the head during sleep, sipping herbal teas, and eating smaller meals can help.
Obesity: Being overweight or obese can put extra pressure on the valves and sphincter that allow acid release.
This is probably why obesity is often associated with acid reflux and GERD.
In eight out of nine studies included in a large review, BMI (body mass index, a measure of body fat) rose, so did GERD symptoms.
The same study review found that obesity was correlated with higher levels of other related disorders, including erosive esophagitis, esophageal and gastric cancers. (15)
Large meals: Eating bigger meals is a culprit, as is snacking too close to bedtime. An overly full stomach places excessive pressure on the diaphragm, causing acid to travel upward.
Smoking cigarettes: This impairs muscle reflexes and increases acid production, and it should be avoided for anyone suffering from acid reflux.
Smoking cessation is associated with significant improvement of GERD/acid reflux symptoms. (16)
Medications and supplements: Certain medications, including ibuprofen, muscle relaxers, blood pressure prescriptions, antibiotics, and aspirin, can cause acid reflux and GERD. Potassium and iron supplements can also aggravate reflux symptoms.
(17) Read warning labels, and discuss alternatives with your physician.
Heartburn: Heartburn can be the first symptom of an H. pylori infection that’s common in two-thirds of the population and tied to stomach ulcers.
Left untreated, severe infection can sometimes contribute to the formation of stomach cancer.
Excessive exercise: Due to taxing the nervous system, overtraining and getting too little rest can cause acid reflux by putting extra pressure on the abdominal cavity.
This includes running and other aerobic high-impact exercises. (18)
Magnesium deficiency: Low magnesium levels may lead to the sphincter’s improper functioning that prevents acid from escaping. (19)
Chronic cough: There is a strong correlation between cough and acid reflux.
Although this relationship is not causal (meaning researchers have not definitely proven one causes the other), the cough may be either a factor in developing GERD or a symptom of the process of acid escaping into the esophagus. (20)
Acid Reflux vs. GERD vs. Heartburn: How Are They Different?
These painful digestive conditions are related and tend to cause similar symptoms; however, they usually develop in stages.
In the case of acid reflux, the patient experiences a backward flow of stomach acid into the esophagus. When this progresses, it can be diagnosed as GERD, which is considered to be more severe. (21)
Heartburn is also commonly called GERD. GERD’s most common symptom is frequent chest and burning sensations (hence the name “heartburn”).
Other GERD signs are difficulty swallowing or keeping down food/liquids (very common in young children), coughing, wheezing, and chest pain. Most often, these symptoms occur at night.
It’s estimated that 60 percent of Americans have heartburn at least once a year, with 20–30 percent suffering at least once a week.
(22) An alarming finding is that the prevalence of weekly heartburn and other symptoms of acid reflux rose nearly 50 percent over the last decade.
Findings from one study conducted over 11 years in Norway found that acid reflux incidence rose from around 11 percent of the population to over 17 percent within this time period. A similar rise has happened in the U.S. and other industrialized countries. (23)
While it might not be the biggest deal to have acid reflux symptoms from time to time, research shows that people with long-standing, chronic heartburn are at greater risk for serious complications, including stricture (narrowing) esophagus and esophagitis, an inflammation of the esophagus.
Conventional Treatments
The three main types of medicines to treat acid reflux symptoms or those caused by GERD are antacids, histamine type 2 receptor antagonists (H2 blockers), and proton pump inhibitors (PPIs).
Should these not work or more serious intervention is needed, doctors will sometimes recommend surgery to tighten the lower esophageal sphincter.
Unfortunately, this surgery is not a cure, and symptoms may return.
The major problem here is the insistence that excessive stomach acidity is the problem.
Your stomach functions optimally when it is between 1.5 and 3.5 pH (an extremely acidic environment), and acid-blocking drugs can raise that pH somewhere around two points (a higher pH means a lower acid level).
What’s the problem with that?
Well, for one, they don’t address the root problem and provide only temporary relief.
When antacids make the stomach less acidic, more acid is automatically produced to bring the stomach back to its intended pH level.
The body will continue this process every time a medicinal measure is taken to reduce acidity.
Hypochlorhydria, the clinical term for low stomach acid, is an under-researched and dangerous condition.
Every time you take antacids, H2 blockers, or PPIs, you contribute more to this problem (which may be one reason you develop heartburn in the first place).
Prolonged hypochlorhydria leads to chronic atrophic gastritis and is associated with side effects, including vitamin B12 deficiency, autoimmune conditions, asthma, diabetes, chronic fatigue, and many other disorders. (24)
Antacids
According to common (and faulty) assumptions about excessive acid levels causing a dangerously high acidity level in the stomach, most practitioners recommend over-the-counter antacids as a first line of defense against heartburn reflux.
A medication such as TUMS® can give quick relief (within a matter of minutes) to a case of heartburn — but, like most conventional medicine, this is used to treat a symptom rather than an underlying disorder.
The side effects of antacids themselves list 20 issues related to repeated use: (25)
- Diarrhea
- Constipation
- Nausea
- Vomiting
- Feelings of discomfort
- Loss of appetite
- Mood/mental changes
- Weakness
- Calcium loss
- Osteoporosis
- Kidney stones
- Wrist/ankle swelling
- Bone pain
- Discolored stool
- Aluminum toxicity
- Slow breathing
- Frequent urination
- Headaches
- Muscle pain
- Drug/supplement interactions
Histamine Type 2 Receptor Agonists (H2 Blockers)
Also available over the counter, H2 blockers work more slowly than antacids to reduce stomach acid and take longer to treat symptoms (60 to 90 minutes) but are intended to last for longer periods of time.
These include Pepcid/Pepcid AC®, Axid®, Tagamet®, and Zantac® and work by blocking a substance in the body that encourages acid production in the stomach.
By stopping the production of hydrochloric acid (HCl, which is your stomach’s natural acid), these medications also stop pepsin production, the digestive enzyme responsible for breaking down protein so it can be digested.
This allows for undigested protein to make its way to your intestines, further increasing intra-abdominal pressure (a possible underlying cause of acid reflux/GERD).
Raising your stomach’s pH beyond what it was intended for also increases your risk of infection, as the bacteria that would be killed by a healthy pH of 3 in the stomach can live when they should not.
(26) Users run the risk of infection by common bacteria like listeria and salmonella and are at a higher risk of developing pneumonia, tuberculosis, typhoid, and dysentery. (27, 28)
H2 blockers have several drug interaction warnings and might cause the following side effects, especially when taken in large doses over time:
- Headaches
- Anxiety
- Depression
- Mental disturbances
- Diarrhea
- Dizziness
- Rash
- Headache
- Impotence
- Breast enlargement in men
- Confusion
- Hallucinations
- Heart issues
- Kidney problems
- Upset stomach
- Vomiting
- Constipation
- Cough
- Liver damage
- Stomach cancer (in people with untreated H. pylori infection)
- Pneumonia (in hospitalized patients, the elderly and children) (29)
- Ulcer perforation and bleeding
- Iron deficiency (30, 31)
- Decreased folate absorption (32)
- Calcium deficiency (33)
- Decreased zinc absorption (34)
Proton Pump Inhibitors (PPIs)
The most dangerous class of conventional acid reflux drugs is known as proton pump inhibitors.
These medications (17 are on the market, at current count) control acid reflux symptoms by permanently blocking an enzyme that tells your stomach to produce acid, H+/K+ ATPase, found in the parietal walls of the stomach lining.
Popular PPIs include Nexium®, Aciphex®, Prevacid®, and Prilosec®.
Recent releases by the media have shown the reason for concern about taking PPIs, especially in the long-term.
The FDA has released warnings about PPIs in the last several years regarding magnesium deficiency, increased risk of bone fractures, and C. diff-related diarrhea.
Since they act like “super” versions of the above two classes of drugs in many ways, the same associated side effects are commonly found in this medication class. Indeed, it seems like PPIs might induce the very issues they seek to correct.
(35) There are also many other researched problems and side effects of PPIs, leading to the understanding of many that these medications should not be used for extended treatment. (36)
C. difficile: This bacterial infection is a potential danger for those taking both H2 blockers and PPIs.
Researchers at McGill University in Quebec found an increase of C. diff infection risk of two times for those taking H2 blockers and nearly three times for PPIs. (37)
Small Intestinal Bacterial Overgrowth (SIBO): One study found an increase of SIBO at a rate of 50 percent in patients on PPIs versus 6 percent in the control group. (38)
Vitamin B12 deficiency: Patients on PPI drugs do not properly absorb many vitamins and minerals. Most notably is the discovery that vitamin B-12 is particularly problematic for these people.
(39, 40) A deficiency in B12 can lead to chronic fatigue, muscle pain/weakness, memory and mood changes, heart palpitations, and digestive issues, among other symptoms.
Stomach cancer: Because it increases secretion of the hormone gastrin, a PPI drug like Prilosec® can result in three to 10 times the amount of gastrin normally found in the human body.
(41) Hypergastrinimia (large concentrations of gastrin) is associated with higher rates of gastric cancer. (42)
Ulcers: Duodenal (intestinal) and gastric ulcers may be another result of long-term PPI usage.
H. pylori cause ninety percent of duodenal ulcers and 65 percent of gastric ulcers. One experiment found that H. pylori infection couldn’t happen without using acid-lowering drugs first to raise the stomach’s pH. (43, 44)
Inflammatory bowel conditions: PPIs can decrease extracellular levels of adenosine, which plays a big role in inflammatory processes within the digestive system.
(45, 46) Because of this, it’s possible that digestive issues caused by inflammation, such as Crohn’s disease, ulcerative colitis, and IBS, may be caused or exacerbated by PPI intake.
Irritable bowel syndrome (IBS) is also associated with SIBO, which I’ve already shown as a potential complication of acid reflux.
Leaky gut: Proton pump inhibitors affect the permeability of the gastric lining, which can, in turn, lead to a leaky gut. This condition is associated with mood issues, autoimmune diseases, and many other health problems.
Asthma: GERD and asthma are closely related — it’s estimated that about 80 percent of asthmatics suffer from GERD.
(47) The escape of acid into the esophagus causes a drop by tenfold in the ability to allow air into the lungs, resulting in a much higher level of reflux for asthma patients. (48)
Arthritis: People taking NSAIDs (non-steroidal anti-inflammatory drugs) like aspirin or acetaminophen to treat arthritis pain develop gastrointestinal issues like ulcers much more often than the average person.
(49) NSAIDs block a protective enzyme that is meant to protect the lining of the stomach.
Ultimately, combining these medications can result in even faster degradation of the stomach lining and cause more ulcers.
A Stanford study found that not only did the PPIs not decrease gastrointestinal symptoms, but they also actually resulted in double the number of hospitalizations from complications.
Death: A review conducted in St. Louis was released in July 2017 regarding a five-year observation of patients on H2 blockers and PPIs, finding that the long-term PPI users were at more risk of death.
These results increased in significance based on the duration a person had been taking PPIs. (50)
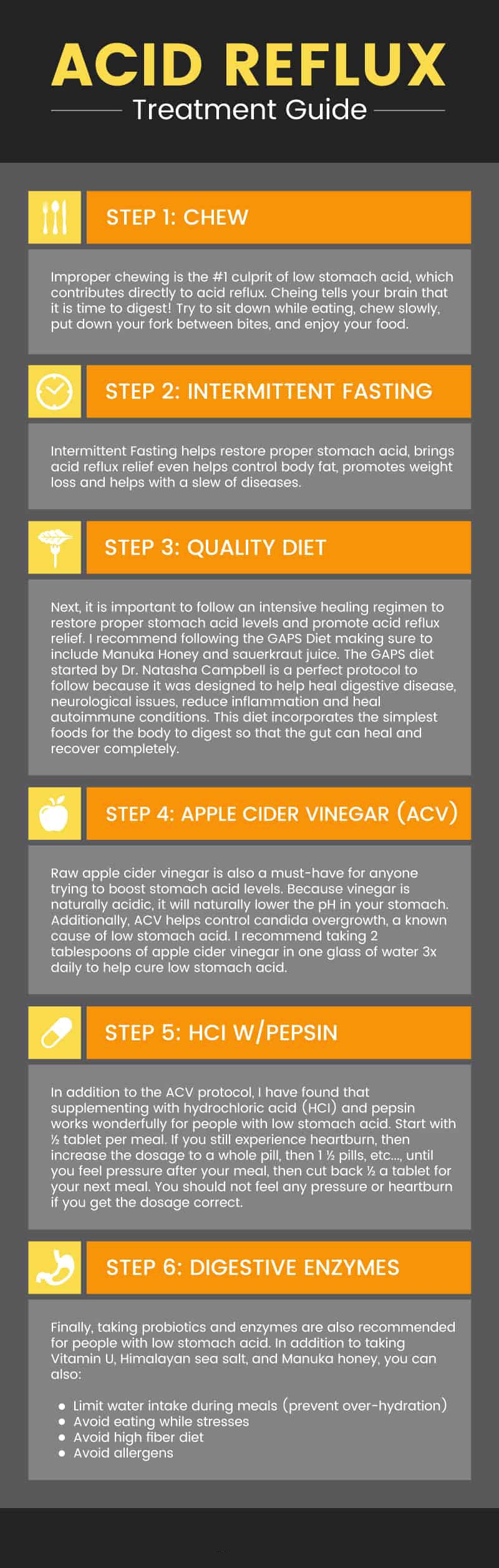
Natural Remedies for Acid Reflux Symptoms
1. Acid Reflux Diet
Virtually every research study done on GERD and acid reflux points to diet as a contributing factor.
First and foremost, acid reflux symptoms and GERD must be treated by changes in your diet to avoid long-term complications and restore healthy digestive function.
Don’t ignore your body trying to alert you to a problem in your digestive tract.
For good digestive health and overall health and wellness, it’s important to select unprocessed, organic foods free from GMOs as much as possible. Increasing fiber intake, supporting healthy bacteria in your gut with probiotic-rich foods, and taking supplements if necessary can help resolve symptoms.
Other steps include reducing grains (especially when refined) and sugar consumption, eating high-quality protein, and reducing refined vegetable oils.
All of this helps protect the GI tract, balance hormonal function, and help prevent many serious chronic diseases associated with poor digestive health.
Here are some foods that tend to make acid reflux worse and therefore should be avoided to minimize symptoms:
- Alcohol
- Carbonated beverages, sugary drinks, or energy drinks
- Artificial sweeteners
- Fried foods
- Vegetable oils, including canola oil
- Spicy foods
- Processed foods
Foods that can help improve acid reflux include fresh organic vegetables (especially leafy greens, squash, artichoke, asparagus, and cucumbers);
free-range chicken and grass-fed beef; probiotic foods like yogurt; bone broth; and healthy fats like coconut or olive oil.
Apple cider vinegar, aloe vera, parsley, ginger, and fennel are also helpful. (51)
2. Supplements for Acid Reflux Symptoms
Besides eating a healthy diet of foods that help to soothe acid reflux and GERD symptoms, some find improvements when adding natural supplements to their diets. These can include:
Digestive enzymes — Take one or two capsules of a high-quality digestive enzyme at the start of each meal. Digestive enzymes help foods fully digest and nutrients absorb properly.
Probiotics — Take 25–50 billion units of high-quality probiotics daily. Adding healthy bacteria helps balance the digestive tract and crowd out bad bacteria that can lead to indigestion, leaky gut, and poor absorption of nutrients.
HCL with Pepsin — Take one 650 milligram pill before each meal. Add additional pills as necessary to keep uncomfortable symptoms at bay.
Chamomile, papaya, or ginger herbal tea — Sip one cup of chamomile tea before bed, sweetened with raw honey. Chamomile tea helps reduce inflammation in the digestive tract, supporting healthy functioning. You can also boil a one-inch piece of fresh ginger in 10 ounces of water for 10 minutes. Also, papain, an enzyme in papaya, aids in digestion by breaking down proteins.
Magnesium complex supplement — I recommend taking 400 milligrams of a high-quality magnesium supplement twice per day.
Apple cider vinegar — Although no official studies have been conducted on the impact of apple cider vinegar on acid reflux and GERD, anecdotal evidence seems to support that it can be an incredible natural remedy for acid reflux.
3. Other Tips for Improving Digestive Health
- Raise the head of the bed four to six inches. Use blocks to raise the bed, not just a pillow to keep your head propped up, helping keep acid in the stomach.
- Exercise and manage stress. A sedentary lifestyle and stress worsens symptoms of acid reflux and overall disrupt digestion. Try yoga, meditation, acupuncture, art or music therapy, or whatever helps you effectively manage stress.
- Don’t overeat. Eat smaller meals to properly digest foods, as large meals and overeating put extra pressure on the sphincter.
- Give up smoking and drinking too much alcohol.
- Don’t consume food three hours before bed. Allow your stomach to digest the foods from the meal, and sip an herbal tea instead.
- Chew foods more thoroughly. Most people today don’t chew their food enough. Remember, digestion starts in the mouth.
Precautions
If your acid reflux symptoms interfere with your lifestyle or daily activity and last for more than two weeks, then consider visiting a doctor.
Other reasons to get a professional opinion on treatment options include experiencing hoarseness; worsening of asthma after meals; pain that’s persistent when lying down; pain following exercise; difficulty breathing that occurs mainly at night; and trouble swallowing for more than one to two days.
To determine a GERD diagnosis, doctors may perform an endoscopy, a procedure involving a small tube inserted into the throat to look at the esophagus, stomach, and small intestine condition.
Some evidence indicates that an endoscopy may not be as effective as previously hoped, but it is still common.
Another method of detecting acid reflux/GERD when a patient complains of acid reflux symptoms is the barium swallow test.
A barium solution is ingested, allowing for internal X-rays to locate esophageal changes. Unfortunately, only 1 out of 3 GERD patients have noticeable esophageal changes that can be seen on a barium swallow X-ray.
One more diagnostic is a stomach acid test in which the stomach contents are emptied, and gastrin is injected into the body to determine acid secretion. (52)
If you are concerned you may have low stomach acid, most doctors will not recommend testing (because low stomach acid isn’t the traditionally accepted cause of acid reflux symptoms). Still, you can personally ask for a Heidelberg test.
Key Points
- Acid reflux is caused by stomach acid creeping up into the esophagus. Acid reflux symptoms usually include chest pains, heartburn, a bad taste in the mouth, bloating, gas, and difficulty digesting and swallowing properly.
- Common causes of acid reflux and GERD include pregnancy, history of Hiatal hernias, obesity, eating an unhealthy diet, older age, and an imbalance of stomach acid.
- Conventional medicine recommends three levels of acid-blocking medications to treat acid reflux symptoms: antacids, H2 blockers, and PPIs. These medications are associated with many dangerous side effects and do not treat the root cause of acid reflux/GERD.

 Acid Reflux Symptoms
Acid Reflux Symptoms