Embolism Definition Medical
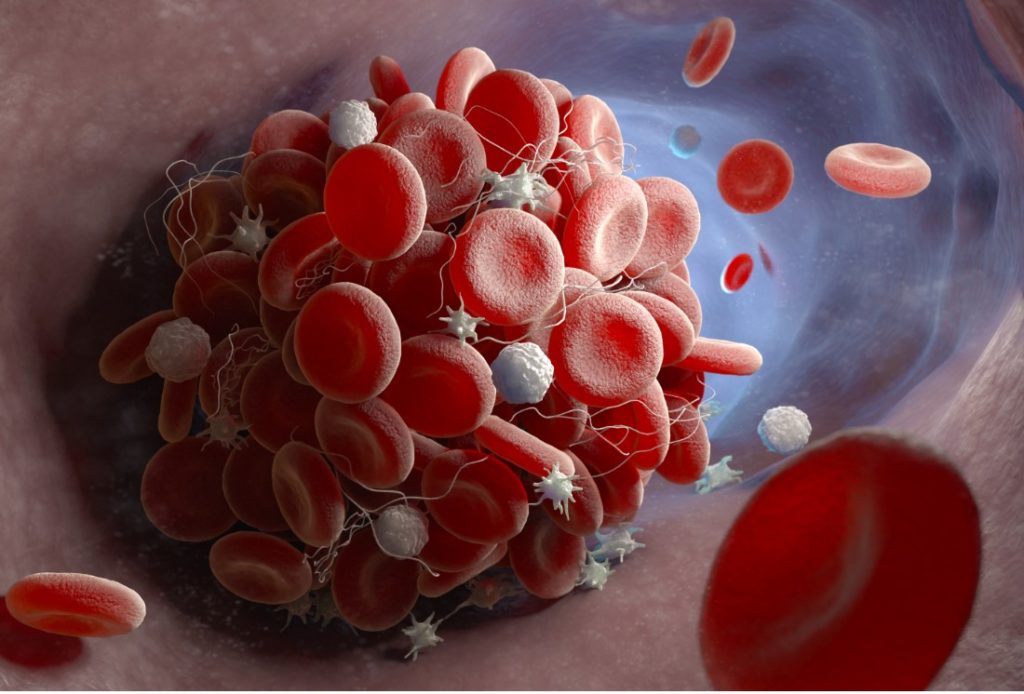
When a blood clot appears inside a blood vessel, it is called a thrombus, and when the clot travels or blocks circulation within a blood vessel, it creates an embolism, a serious medical condition.
Several things can cause blood clots. The most common reasons people get them include injuries like broken bones, muscle tears, or deep bruises.
Other causes include extended periods of inactivity such as long air flights, serious illnesses that keep a person in bed for a long while, and treatments for diseases like cancer that may make the blood clot more easily.
When an embolism forms, it can travel inside larger blood vessels to smaller vessels inside vital organs like the heart, lungs, or brain.
Once the embolism reaches blood vessels that lead to these organs or gets inside the organ, it can prevent blood flow and cause damage to that organ. In some cases, an embolism can be fatal.
TYPES OF EMBOLISM
There are several types of embolism, including:
Pulmonary embolism
This is an embolism in the lung. The blood clot generally forms in an extremity, usually the leg, and travels through blood vessels to the lung.
The most prevalent type of blood clot in the leg is deep vein thrombosis (DVT).
The main symptom of a pulmonary embolism is shortness of breath, but individuals who have this type of embolism may also experience symptoms like:
- weak pulse
- rapid heartbeat
- chest pain that may radiate to arms, neck, or jaw
- blue-tinged skin, especially around lips and fingernails
- anxiety or restlessness
- rapid breathing or panting
- coughing up bloody spit
A pulmonary embolism is a medical emergency. Anyone experiencing one or a couple of these symptoms should seek medical care immediately.
Diagnosing a pulmonary embolism may be difficult, but there are several ways doctors can test for this type of embolism, such as:
D-dimer test—As blood clots break down, they release fragments of a protein called d-dimer. This test measures d-dimer in the blood. If it’s present, it means there is or has been a blood clot.
Imaging tests of the lungs—Chest X-ray, computed tomography (CT) scan, or magnetic resonance imaging (MRI) can all provide images of the lungs to see if there’s damage or a clot.
Pulmonary angiography—This test uses dye, a catheter (small tube), and X-rays to see the pulmonary artery and lungs, looking for the embolism and any damage.
Electrocardiography (ECG)—This test records the heart’s electrical signals and can show if there are certain types of injuries.
Duplex venous ultrasound—This test uses radio waves to create images of the leg’s blood vessels.
Venography—This is a particular type of X-ray of the leg’s vessels that can show blood clots.
Treatment for a pulmonary embolism involves preventing new clots from forming and shrinking existing clots. Medications like blood thinners or clot dissolvers may be prescribed.
Another treatment option is surgery using a catheter to remove the embolism or to install a filter in a large blood vessel in the leg. The filter helps stop blood clots before they can travel to the lungs.
Brain embolism
As the name suggests, a brain embolism (cerebral embolism) is a blood clot that travels to the brain. A brain embolism is a serious medical emergency.
These clots can cause a stroke or a transient ischemic attack (TIA), a mini, temporary stroke.
There are many symptoms of brain embolism and stroke. Specific symptoms experienced will depend on where in the brain the embolism is and where the stroke occurs.
According to the American Stroke Association, an easy way to recognize symptoms of stroke and to know when to call 911 for suspected stroke is “FAST“:
“F”—Face Drooping—Is one side of the face drooping or numb? Have the person smile to see if the smile is crooked.
“A”—Arm Weakness—Is one arm weak or numb? Have the person raise both arms. Does one arm sink?
“S”—Speech—Is the person’s speech slurred? Can they speak? Are they hard to understand? Have them repeat a simple sentence.
“T”—Time to Call 9-1-1. If an individual has these symptoms, even if they stop, call 9-1-1.
Other symptoms of a stroke (caused by a brain embolism) may include:
- difficulty understanding words
- temporary paralysis or all or part of the body or weakness or paralysis on a single side of the torso or face
- inability to recognize things, blurred vision, or blindness
- trouble walking or stiff muscles
- confusion, dizziness, fainting, fatigue, or difficulty staying awake
- difficulty swallowing, nausea, or vomiting
A cerebral or brain embolism is a medical emergency. Anyone with any of these or symptoms should seek medical care immediately.
A brain embolism is diagnosed with similar tests as those used to identify a pulmonary embolism. These tests include imaging tests of the brain such as X-ray, CT scan, MRI, cerebral angiography, or cerebral arteriogram.
Quick treatment for a stroke is imperative. The faster blood flow is returned to the brain, the minor damage occurs. Medication is the most common treatment.
These medications dissolve the clot so blood flow can be restored. Medications may be oral or delivered through a catheter inserted near the clot.
An embolism may also be removed through a catheter. According to the American Heart Association (AHA), medication should be started within 3 hours of the first stroke symptom for the best result.
Retinal embolism
Retinal embolisms can happen if a blood clot that is too small to block larger vessels in the body travels to the eye and stops any tiny blood vessels that feed the retina.
If this happens, it causes an eye stroke, called a central retinal artery occlusion (CRAO), leading to sudden blindness in the affected eye.
In addition to the loss of vision, other symptoms of retinal embolism include:
though often painless, some people have eye pain, headache, fever, jaw, or scalp pain fatigue.
To diagnose an embolism or stroke in the eye, an ophthalmologist, a doctor specializing in eye surgery and eye care, will examine the eyes.
Using medicated drops, the doctor will dilate the eyes to make it easier to see the retina and optic nerve.
The doctor will check a detailed medical history and note any other conditions, like high blood pressure, diabetes, or heart disease.
The primary treatment for retinal embolism is a medication, corticosteroids which help reduce swelling and improve circulation.
The doctor may also prescribe drugs to help lower the pressure in the affected eye. While medication may improve vision slightly, there is currently no medication that can regrow fibers in the retina once they are injured after an embolism.
Other treatment options include hyperbaric oxygen therapy and removing a small amount of fluid from the eye, which may reduce pressure in the eye.
Even after treatment, most people will permanently lose some or all vision in the affected eye.
Septic embolism
A septic embolism happens when an infection causes blood clots to form in the blood. These clots may then travel anywhere in the body, causing injuries like stroke.
A septic embolism threatens the body in two ways, by spreading infection and by blocking blood flow.
Symptoms of septic embolism are similar to signs of infection, and effects vary based on where the embolism forms and travels.
A septic embolism can affect any part of the body.
Symptoms may include things like:
- fever
- chills
- pain
- swelling and inflammation
- dizziness
- cold symptoms like cough and sore throat
- shortness of breath
A septic embolism is diagnosed by blood tests, much like other infections. Other tests may be needed to help assess parts of the body affected by a septic embolism, such as chest X-ray, CT scan, MRI, heart scans (echocardiogram), and ultrasound.
Treatment for septic embolism will depend on where the embolism travels and what infection it causes. The primary treatment is antibiotics.
The doctor may need to drain any pockets of infected fluid called abscesses. Treatment may also include corrective surgery if the infection affects things like areas where artificial limbs come into contact with the body and parts of vital organs like heart valves.
Amniotic embolism
An amniotic embolism occurs during pregnancy when amniotic fluid, the fluid that surrounds a fetus in the uterus, thickens and a clot forms.
These clots can travel within the mother’s body. Depending on where an amniotic embolism travels, it can cause lung damage (pulmonary amniotic embolism) or stroke if the amniotic embolism travels to the brain.
An amniotic embolism can happen suddenly and maybe a medical emergency.
Symptoms include:
- feelings of doom or impending death
- anxiety
- shortness of breath
- low blood pressure, fluid in the lungs
- blood clots
- bleeding from the uterus or cesarian section incision
- rapid heartbeat
- heart failure
- seizures
- loss of consciousness
- fetal distress like abnormal fetal heart rate
To diagnose an amniotic embolism, doctors may perform lab tests like blood tests that can detect clots’ presence, examinations that evaluate the heart and lungs’ health.
Doctors may request imaging tests like chest X-rays and echocardiograms to evaluate the heart.
Treatment of an amniotic embolism will often be emergency care since the embolism may be in the lungs, brain, or heart.
Treatment may include inserting a breathing tube or placing a catheter to help deliver medication and remove the embolism if possible. Medication may be used to help maintain blood pressure and dissolve the clot, and blood transfusion may be necessary.
The fetus may be delivered if possible, and the delivery may be an emergency C-section, a faster, surgical delivery.
Air embolism
An air embolism occurs when gas bubbles form in the blood and block a blood vessel. If the bubble is in a vein, it’s called a venous air embolism.
If it’s in an artery, it’s called an arterial air embolism. An air embolism, much like a blood clot, can travel to the brain, heart, or lungs and can be fatal.
However, an air embolism is very rare.
Several things can cause an air embolism; SCUBA divers can develop them if they are diving in deep water and ascent to the surface too fast.
This has been called “the bends.” Other ways an air embolism can develop include injections, surgery, trauma from an explosion, and lung injuries.
Symptoms of an air embolism will bank on where the embolism travels and will be similar to blood embolisms in that area.
Diagnosing an air embolism first begins with assessing an injury or situation that could have caused an air embolism.
Imaging tests like ultrasound, CT scans may also be ordered to locate and identify an air embolism.
Doctors also monitor patients very closely during surgery to help prevent an air embolism from forming in the first place.
Treatment for air embolism will also depend on where the embolism travels. It may be similar to the treatment for an embolism caused by a blood clot.
Fat embolism
A fat embolism happens when a piece of fat from inside a blood vessel travels to a small vessel and blocks it.
An embolism caused by fat will usually dissolve on its own and cause no health problems. However, though rare, a fat embolism caused by a traumatic break in one of the large bones may lead to fat embolism syndrome (FES), which can cause inflammation and injury to major organs in the body.
Treatment usually includes oxygen and supportive care.
Symptoms of a fat embolism range from none to coma. If severe symptoms are going to occur, they usually appear within two to three days.
These symptoms may occur throughout the body and may include:
- shortness of breath
- rash composed of tiny dots called petechiae
- confusion
- fatigue
- bleeding just under the skin
- anemia
- coma
Several events may cause an embolism.
An embolism can be a life-threatening medical emergency, especially if it involves the lungs or brain.
Knowing the symptoms and when to seek emergency care is essential. In many cases, medical treatment for an embolism is very effective.
Resources
Websites
“Embolism.” MedBroadcast. https://medbroadcast.com/condition/getcondition/embolism (accessed March 1, 2021).
“Embolism.” National Health Service. February 17, 2020. https://www.nhs.uk/conditions/embolism/ (accessed March 3, 2021).
“Pulmonary Embolism.” MedlinePlus. December 8, 2020. https://medlineplus.gov/pulmonaryembolism.html (accessed March 1, 2021).
“Stroke Symptoms.” American Stroke Association. https://www.stroke.org/en/about-stroke/stroke-symptoms (accessed March 1, 2021).
“Understanding Blood Clots.” Centers for Disease Control and Prevention. February 7, 2020. https://www.cdc.gov/ncbddd/dvt/understanding-blood-clots-infographic.html (accessed March 1, 2021).
Organizations
American Heart Association, 7272 Greenville Ave., Dallas, TX, 75231, (800) 242-8721, https://www.heart.org/en .
American Lung Association, 55 W. Wacker Drive, Suite 1150, Chicago, IL, 60601, (800) 586-4872 (LUNG USA), Info@Lung.org, https://www.lung.org/ .
National Blood Clot Alliance (NBCA), 267 Kentlands Boulevard, #2025, Gaithersburg, MD, 20878, (877) 462-2568 (NOCLOT), (703) 935-8845, info@stoptheclot.org, https://www.stoptheclot.org/ .