LUPUS
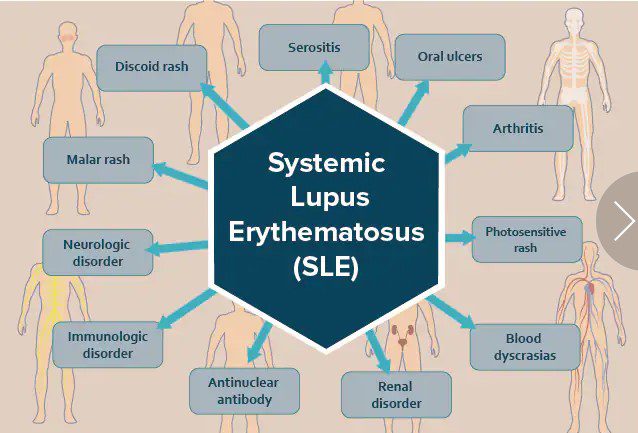
Systemic lupus erythematosus (SLE), ordinarily called lupus, is a chronic autoimmune disease that causes inflammation in many body organs, including the joints, skin, kidneys, lungs, heart, and brain.
It can cause mild to severe symptoms that come and go in waves (called flares).
Despite there is no cure for lupus, treatments continue to improve and allow people with the illness to live better.
There are four types of lupus: SLE (the most common), cutaneous lupus erythematosus (only the skin symptoms of SLE), drug-induced lupus erythematosus, and neonatal lupus (a rare, short-term condition that affects babies born to women with lupus).
PREVALENCE AND STATISTICS
According to the research done by the Lupus Foundation of America, at least five million people have a form of lupus worldwide, including 1.5 million Americans as of 2012.
An estimated 16,000 new people are diagnosed with lupus each year. In industrialized countries, lupus has become 10 times more common over the past 50 years; it is not well understood why lupus is becoming more common.
Lupus more commonly affects women than men. In fact, 90% of adults with lupus are women.
The disease most often affects people ages 15 to 45 years old but may also affect children and younger teenagers.
Lupus is more prevalent in African Americans and people of American Indian and Asian descent.
The illness is two to three times more prevalent in women of color than Caucasian women. For example, one in 537 young African American women has lupus.
Women of African descent also tend to develop lupus younger, have more serious complications, and have higher mortality rates from the disease.
A person with a family history of lupus or other autoimmune diseases may be more likely to develop lupus; 20% of lupus patients have a parent or sibling with lupus.
About 5% of children born to a parent with lupus will develop the disease.
People with lupus may also be more prone to having other autoimmune diseases. In fact, one in three lupus patients also has at least one other autoimmune disease.
LUPUS CAUSES
Even though the cause of lupus is not well understood, a variety of factors are thought to switch on the immune system to overreact, leading to the disease.
Possible factors include:
- Sex: the risk of developing lupus seems to be related to the number of X chromosomes as women (XX), women with an extra X chromosome (XXX), and men with Klinefelter syndrome (XXY) seem to develop lupus more than men (XY)
- Genetics: dozens of genetic variants are known to cause lupus and impact symptom severity; most of the genes associated with lupus affect immune system controls
- Family history: lupus, like other autoimmune diseases, tends to run in families; the inheritance pattern of lupus is unknown.
- Infectious diseases: exposure to certain viruses (such as Epstein-Barr virus)
- Environmental: Diet, stress, smoking, certain medications, sunlight
LUPUS SYMPTOMS
Lupus symptoms range from mild to severe, may only affect one area of the body, and change over time. Initial symptoms may include:
- Fatigue
- Malaise (an overall feeling of discomfort or illness)
- Fever
- Loss of appetite
- Weight loss
- Unexplainable rash
Other symptoms may include:
- Headaches
- Dizziness
- Dry eyes
- Chronic pain
- Muscle pain and weakness
- Stomach pain
- Shortness of breath
- Arthritis (painful, swollen joints and morning stiffness)
- Swollen glands
- Swelling around the eyes
- Leg swelling
- Painless rashes (especially a butterfly-shaped rash on the face over the cheeks and nose)
- Skin lesions that worsen with sun exposure
- Calcinosis (calcium deposits under the skin)
- Vasculitis (damaged blood vessels)
- Petechiae (tiny red spots on the skin)
- Painless sores in the nose and mouth
- Alopecia (hair loss)
- Raynaud’s phenomenon (fingers and toes turning blue-purple, white, or red due to cold or stress)
- Depression
- Confusion
- Cognitive impairment
- Seizures
Symptoms tend to occur in waves when symptoms are present (flares) and absent (remission).
Flares can be mild to severe and tend to be sporadic, not following a pattern. External factors may also worsen symptoms; the butterfly rash may be worsened by exposure to sunlight.
Complications
Lupus may also affect the kidneys, heart, or lungs, causing serious complications:
- Lupus nephritis: inflammation of the kidneys that may require dialysis or a kidney transplant. About one-third of lupus patients develop nephritis.
- Brain and nervous system inflammation, causing headaches, confusion, memory problems, and strokes.
- Blood vessel inflammation, causing high fevers, behavioral changes, and seizures.
- Pericarditis: infection of the lining tissue around the heart (pericardium).
- Coronary artery disease or hardening of the arteries can lead to a heart attack.
- Atherosclerosis: fatty buildup in the blood vessels. Although it is widespread in the general population, it is even more common in lupus patients.
- Peripheral neuropathy: abnormal sensations and weakness in the limbs.
Lupus can lead to serious complications that can be fatal, such as heart attacks and strokes.
According to the Lupus Foundation of America, 10-15% of lupus patients die prematurely due to complications.
Lupus and pregnancy
If lupus symptoms are under control, most women living with lupus can have healthy pregnancies.
Talk with a doctor while planning a pregnancy and find an obstetrician with experience working with women with lupus.
LUPUS DIAGNOSIS
There is no test for lupus at the time being, and it can be difficult to diagnose because symptoms can be generalized to other diseases and come and go.
According to the Lupus Foundation of America, it takes an average of six years to be diagnosed with lupus after the onset of symptoms. Lupus may be diagnosed using:
- Medical history, family history, and symptoms
- A physical exam
- Laboratory tests
- A skin or kidney biopsy
LUPUS TREATMENT
No cure exists for lupus, but treatment allows many people living with lupus to manage the condition.
Treatments aim to manage symptoms, prevent flares, prevent or slow organ damage, and improve quality of life.
As treatments continue to improve, it is possible to prevent flares that the disease goes into complete remission so effectively.
Medical treatments include:
- Anti-inflammatory drugs (aspirin, acetaminophen, NSAIDs) to treat pain and fever.
- Antimalarial drugs (chloroquine, hydroxychloroquine) treat fatigue, joint pain, skin rashes, and lung inflammation.
- Corticosteroids (prednisone, prednisolone, methylprednisolone) to reduce inflammation throughout the body.
- Immunosuppressants (cyclophosphamide, methotrexate, azathioprine) to calm down the over-reactive immune system.
- Biologics (Belimumab) inhibit certain immune system cells and prevent the immune system from attacking the body.
- Anticoagulants (low-dose aspirin, heparin, warfarin) to prevent blood clots.
Complimentary therapies and lifestyle choices may also help manage or relieve symptoms. However, they may not be thoroughly tested via clinical studies. Therapies and lifestyle choices include:
- Supplements: can be problematic and dangerous; follow your physician’s recommendations on a diet and which—if any—supplements you should take.
- Special diets: eat lots of fruits, vegetables, and whole grains
- Acupuncture
- Exercise
- Quit smoking
- Sun protection: use sunscreen, wear long-sleeved shirts and a hat
- Stress management: meditate, practice deep breathing, do yoga, read.
Resources
Websites
“Lupus.” Centers for Disease Control and Prevention. July 1, 2020. https://www.cdc.gov/lupus/index.htm (accessed March 1, 2021).
“Lupus.” Mayo Clinic. January 21, 2021. https://www.mayoclinic.org/diseases-conditions/lupus/symptoms-causes/syc-20365789 (accessed March 1, 2021).
“Lupus.” National Institutes of Health: National Center for Advancing Translational Sciences—Genetic and Rare Diseases Information Center (GARD). August 9, 2017. https://rarediseases.info.nih.gov/diseases/10253/lupus (accessed March 1, 2021).
“Systemic lupus erythematosus.” MedlinePlus Genetics. August 18, 2020. https://medlineplus.gov/genetics/condition/systemic-lupus-erythematosus/ (accessed March 1, 2021).
“Systemic Lupus Erythematosus (Lupus).” National Institute of Arthritis and Musculoskeletal and Skin Diseases. June 2019. https://www.niams.nih.gov/health-topics/lupus (accessed March 1, 2021).
“What is systemic lupus erythematosus (SLE)?” Lupus Foundation of America. December 2, 2020. https://www.lupus.org/resources/what-is-systemic-lupus-erythematosus-sle (accessed March 1, 2021).
Organizations
Lupus Foundation of America, 2121 K Street NW, Suite 200, Washington, DC, 20037, (202) 349-1156, Fax: (202) 349-1156, info@lupus.org, https://www.lupus.org/ .
Lupus Research Alliance, 275 Madison Ave, 10th Floor, New York, NY, 10016, (800) 867-1743, (212) 218-2840, info@lupusresearch.org, https://www.lupusresearch.org/.
National Institute of Arthritis and Muscoloskeletal and Skin Diseases (NIAMS), 31 Center Dr, MSC 2350, Bethesda, MD, 20892-2350, (877) 226-4267, (301) 565-2966, Fax: (301) 718-6366, NIAMSinfo@mail.nih.gov, https://www.niams.nih.gov/ .